Chronic Bladder Infections
(Recurring Bladder/UTI Infections)
The root of your chronic bladder infections can be treated naturally & effectively with homeopathy & integrative medicine.
Chronic Bladder Infections:
Natural Therapies & Treatment
Many women will experience only a couple of urinary tract infections in their lifetime. However, 45-50% of women will suffer new infections every six months - sometimes even more frequently. This can be exhausting both physically and emotionally.
Recurring urinary tract infections can be challenging to treat, as there are a few factors that need to be addressed simultaneously in order to help break the cycle.
Bacteria overgrowth is often present (typically strains of E. coli) as well as inflammation of the bladder caused by a biofilm, which impacts the immune system’s ability to help get rid of underlying infections. Hormonal imbalance is also a factor that plays a critical role in recurring bladder infections.
By using homeopathic medicines and nutritional supplements, I can help balance your hormones and improve your immune system’s response to help break this cycle of chronic urinary tract infections.
Homeopathy & Nutraceutical (supplements) for Chronic Bladder Infections
What are chronic bladder infections?
Chronic urinary tract infections occur when you have more than one infection within six months. Unfortunately, some women are more prone to recurrent urinary tract infections due to a wide range of factors.
Each woman’s symptoms and experiences with chronic urinary tract infections can vary from one another, but some common symptoms are:
Frequent urination
Burning or tingling sensation while urinating
Pain in bladder region
Discomfort in pelvic region
Pain in mid to lower back (kidneys)
Fatigue

What causes chronic bladder infections (chronic UTI)?
A healthy bladder and urinary system never contain bacteria. When a woman has a urinary tract infection, this means bacteria (commonly E. coli) has entered the urinary system through the urethra and multiplied. When a woman is experiencing a new bladder infection every six months, this usually means the bacteria has found a way to make itself very hospitable within her bladder.
Some of the causing factors include inflammation of the bladder, bladder biofilm and hormone imbalance, which impacts the immune system’s ability to break the cycle of chronic urinary tract infections. Read more about these factors below.
Chronic Inflammation of the Bladder
Bladder inflammation (also known as cystitis) is a common complication of a bladder infection. The lining of the bladder can become irritated and inflamed, often as a result of a bacterial infection.
Bladder inflammation can cause symptoms such as:
Frequent urges to urinate
Pain or burning during urination
Discomfort or pain in the lower abdomen
In some cases, bladder inflammation can damage the lining of the bladder, making it more susceptible to recurrent infections. This inflammation can also cause scarring and thickening of the bladder wall, which can obstruct the flow of urine and make it easier for bacteria to grow.
Treatment for chronic bladder inflammation not only requires resolving the bacterial infection, but reducing inflammation as well.
If the bladder develops chronic inflammation, the inflammation that helps heal the infection can then become inflammation that contributes towards recurring infections. This inflammation causes the bladder membrane to help the bacteria thrive inside the bladder wall, resulting in the development of biofilm.
Host restriction of Escherichia coli recurrent urinary tract infection occurs in a bacterial strain-specific manner Valerie P. O’Brien Denise A. DorseyThomas J. Hannan Scott J. Hultgren
The Role of Biofilms in Chronic Bladder Infections
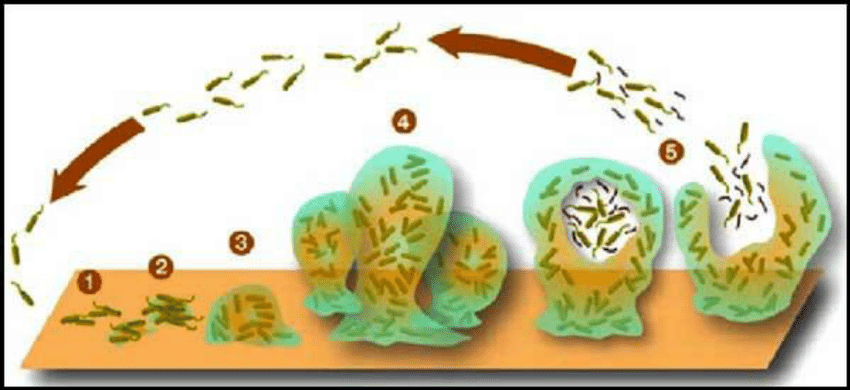
Biofilms are thin layers of bacteria that can form on the surface of the bladder and other areas of the urinary tract.
Bacteria attach to the bladder wall, creating a biofilm and releasing chemicals that improve the biofilm’s ability to stay inside the bladder wall (also know as an adhesion). These biofilms are typically composed of different types of bacteria that fight the body's immune system and antibiotics.
Biofilms provide a safe haven for bacteria to grow and multiply. Once formed, a biofilm can be difficult to eradicate, even with antibiotics. This can lead to recurring bladder/urinary tract infections, as the bacteria in the biofilm can continue to wreak havoc even after treatment.
Treatment for chronic bladder infections that are caused by biofilms often requires breaking down the biofilm and killing the bacteria. This means addressing inflammation, improving the immune system function and balancing hormones.
Biofilm Formation (image © Creative Commons Library).
Hormones and its Role with Chronic Bladder Infections
Healthy levels of estrogen can improve bladder health & natural immune defense
Estrogen has been shown to have a protective effect on the urinary tract. Low levels of estrogen have been linked to an increased risk of urinary tract infections (UTIs). Estrogen helps to maintain the acidity of urine, which can kill bacteria and prevent infections. Additionally, estrogen helps promote the growth of good bacteria in the urinary tract, which can help to keep harmful bacteria in check.
Clinical evidence shows that a drop in estrogen before and during menstruation can cause a dramatic shift in both the urinary microbiome and the immune system. This can result in an increased susceptibility to urinary tract infections. Estrogen also plays a vital role in helping regulate the immune system and maintaining healthy flora levels in the vaginal and digestive tract.
Women who are going through menopause often experience a natural decline in their levels of estrogen, increasing their risk of developing chronic UTIs.
Having a healthy balance of estrogen is important, as it helps the bladder wall regulate inflammation and prevents bacteria from entering.
In Science Translational Medicine (Vol. 5, Issue 190).
Both estrogen and progesterone are hormones that play a role in many bodily functions, including the development and maintenance of the reproductive system. In women, estrogen and progesterone levels naturally fluctuate throughout the menstrual cycle and during pregnancy.
Natural Treatment Options for Chronic Bladder Infections A Modern Holistic Approach Using Homeopathy & Nutraceuticals
There are 4 steps we take to help you with bladder infections:
Step 1 - Assess lifestyle, emotional & physical wellbeing
There are several lifestyle factors that can increase your risk of recurrent bladder infections. One of these factors is not drinking enough fluids (especially water), which can lead to dehydration. This concentrates the urine, making it more hospitable for bacterial growth.
Intercourse, pregnancy, menopause and certain medical conditions (such as diabetes or a weakened immune system) are factors that can also increase the risk of recurrent bladder infections.
Step 2 - Address Clinical Symptoms
People living with recurrent bladder infections often experience a reduced quality of life. The good news is that I can provide relief for your symptoms quite quickly. This allows you to experience positive results and reduced symptoms, while we simultaneously work to treat any underlying factors.
Step 3 - Reduce Inflammation & Biofilm
Your treatment plan is designed to help not only reduce inflammation inside your bladder, but also help improve your body’s immune system response in restoring your bladder to a healthy state.
The presence of bacterial biofilms may explain why you are struggling to recover from chronic bladder infections. Natural antibacterial treatments can be used to reduce the formation and adherence of these biofilms.
Step 4 - Hormone Balancing (Estrogen & Progesterone)
Balancing hormones, especially progesterone and estrogen, may help reduce the risk of developing chronic bladder infections.
Progesterone can cause changes in the urinary tract that make it more susceptible to bacterial infections. On the other hand, estrogen can help strengthen the muscles in the urinary tract and help prevent infections.
Balancing these hormones can help you maintain a healthy urinary tract and reduce the risk of chronic bladder infections.
At Nielsen Clinic, Dr. Vijay Nielsen’s treatment approach is all about understanding your specific health concerns, so I can design a customized treatment plan to help you with chronic/recurring bladder infections. This approach is based on over 17 years of clinical experience and published medical research. Dr. Vijay Nielsen has helped many women suffering from recurring or chronic bladder infections achieve their health goals.
Book an appointment
Are you ready to reclaim your health? It all begins with taking the first step of filling out the form to request an appointment!
It’s important to me to provide guidance and support through a science-based, holistic and integrative approach using homeopathic medicine and nutraceuticals. I will help you identify the root causes of your health issues and develop a plan to address them.
While monitoring your progress and adjust your treatment plan as needed to ensure you achieve your health goals. I will provide information along the way to help you make informed decisions about your own care, while offering support and encouragement to help you stay on track with your health goals.
To your success,
Dr. Vijay Nielsen, DMS HD RAHom-A
Homeopathic Doctor | Registered Homeopath – Calgary, Alberta Canada Integrative Medicine
Sources
Aydin, A., Ahmed, K., Zaman, I., Khan, M. S., & Dasgupta, P. (2014). Recurrent urinary tract infections in women. In International Urogynecology Journal (Vol. 26, Issue 6, pp. 795–804). Springer Science and Business Media LLC.
de Paula Coelho, C., Motta, P. D., Petrillo, M., de Oliveira Iovine, R., Dalboni, L. C., Santana, F. R., Correia, M. S. F., Casarin, R. C. V., Carvalho, V. M., & Bonamin, L. V. (2017). Homeopathic medicine Cantharis modulates uropathogenic E. coli (UPEC)-induced cystitis in susceptible mice. In Cytokine (Vol. 92, pp. 103–109). Elsevier BV. https://doi.org/10.1016/j.cyto.2017.01.014
Ikäheimo R, Siitonen A, Heiskanen T, Kärkkäinen U, Kuosmanen P, Lipponen P et al (1996) Recurrence of urinary tract infection in a primary care setting: analysis of a 1-year follow-up of 179 women. Clin Infect Dis 22(1):91–99
Kawakami, A. P., Osugui, L., César, A. T., Priven, S. W., Carvalho, V. M. de, & Bonamin, L. V. (2021). In vitro growth of uropathogenic Escherichia coli isolated from a snow leopard treated with homeopathic and isopathic remedies: a pilot study. In International Journal of High Dilution Research - ISSN 1982-6206 (Vol. 8, Issue 27, pp. 41–44). International Journal of High Dilution Research - IJHDR. https://doi.org/10.51910/ijhdr.v8i27.341
Nicolle LE (1992) Prophylaxis: recurrent urinary tract infection in women. Infection 20(Suppl 3):S203–S205, discussion S206–S210
Pannek, J., Jus, M. C., & Jus, M. S. (2012). Homöopathische Prophylaxe von Harnweginfekten bei Patienten mit neurogener Blasenfunktionsstörung. In Der Urologe (Vol. 51, Issue 4, pp. 544–546). Springer Science and Business Media LLC. https://doi.org/10.1007/s00120-012-2838-1
Soto, S. M. (2014). Importance of Biofilms in Urinary Tract Infections: New Therapeutic Approaches. In Advances in Biology (Vol. 2014, pp. 1–13). Hindawi Limited.
Stapleton AE, Dziura J, Hooton TM, Cox ME, Yarova-Yarovaya Y, Chen S et al (2012) Recurrent urinary tract infection and urinary Escherichia coli in women ingesting cranberry juice daily: a randomized controlled trial. Mayo Clin Proc 87(2):143–150
Tenke, P., Köves, B., Nagy, K. et al. Update on biofilm infections in the urinary tract. World J Urol 30, 51–57 (2012).